In the United States, about 1 in 10,000 people have urethral stricture disease. This condition makes the urethra narrower, affecting how we urinate1. It can cause a slow, painful flow of urine, frequent infections, and even harm the kidneys if not treated1. Luckily, South Florida offers new treatments, like the Optilume procedure at Z Urology1.
Z Urology in Boca Raton is known for its advanced urology care. They offer the Optilume treatment for urethral strictures1. This method uses the latest technology and Z Urology’s team to help patients in Miami-Dade, Broward, and Palm Beach County1.
Key Takeaways
- Urethral stricture disease is a common condition that narrows the urethra, causing urinary difficulties and potential complications
- Advanced treatment options, such as the Optilume procedure, are now available at Z Urology clinics throughout South Florida
- The Optilume treatment combines innovative technology with expert care to provide a minimally invasive solution for urethral strictures
- Z Urology is a leading urology practice in Boca Raton, dedicated to delivering exceptional care and transformative outcomes for patients
- Patients in Miami-Dade, Broward, and Palm Beach County can access the Optilume treatment at Z Urology’s conveniently located clinics
Understanding Urethral Stricture Disease
Urethral stricture disease is when the urethra, the tube for urine, gets narrower2. This happens because of scar tissue, which blocks urine flow2. It greatly affects how you urinate.
What is a Urethral Stricture?
A urethral stricture is a blockage in the urethra, usually from scarring or inflammation2. It makes it hard to fully empty your bladder. This leads to various urinary problems and serious issues if not treated.
Impact on Urinary Function
Urethral strictures can really mess with your urine flow. You might struggle to pee, have a weak stream, or feel like you’re not fully emptying your bladder2. This can cause infections, damage to your bladder, and even kidney problems if not managed.
Common Risk Factors
Things that increase your risk of getting a urethral stricture include injuries, like pelvic fractures, or medical procedures3. Inflammation from conditions like lichen sclerosus or urethritis also raises your risk3. Knowing these risks helps prevent and treat the condition early.
Quick action on urethral stricture disease can prevent serious problems. It helps keep your urinary system healthy and improves your life quality2.
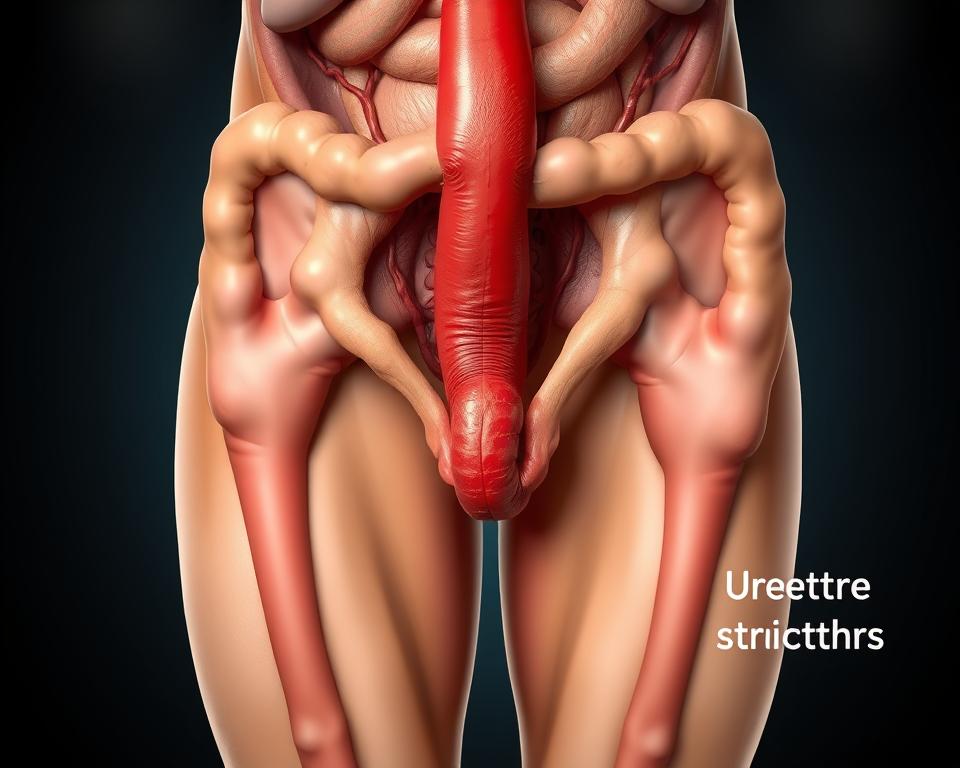
Anatomy of the Urethra and Stricture Formation
The urethra is a narrow tube that carries urine from the bladder out of the body4. It’s key to the urinary system. Knowing its anatomy helps in treating urethra stenosis, urethral blockage, and urethral trauma.
The urethra has different parts, like the prostatic, membranous, and spongy (or penile) urethra5. Narrowings, or strictures, can happen anywhere. This leads to trouble with urination and other issues.
Strictures form when the urethra’s lining gets scarred and narrows, a process called ischaemic spongiofibrosis5. This can occur for many reasons, including:
- Traumatic injuries to the urethra, such as from pelvic fractures or instrumentation
- Medical procedures, like catheterization or surgery, that can damage the urethral tissue
- Inflammatory conditions, such as lichen sclerosus or urinary tract infections
Knowing where and how much a stricture is narrowed is key for treatment5. Tests like retrograde urethrography and ultrasound help see the stricture’s details.
Correctly diagnosing and managing urethral strictures is vital for keeping urine flow normal6. By treating the cause and tailoring care, doctors can help patients with urethra stenosis, urethral blockage, and urethral trauma live better lives.
| Stricture Location | Common Causes |
|---|---|
| Penile Urethra | Iatrogenic, Inflammatory |
| Bulbar Urethra | Idiopathic, Iatrogenic, Traumatic, Inflammatory |
| Posterior Urethra | Traumatic, Iatrogenic |
“Understanding the anatomy of the urethra and the factors that contribute to stricture formation is essential for effective diagnosis and treatment of this condition.”
By tackling the root causes and using modern treatments, doctors can improve urine flow and quality of life for those with urethra stenosis, urethral blockage, and urethral trauma.
Common Causes and Risk Factors for Urethral Strictures
Urethral strictures come from many sources, each with its own problems. Traumatic injuries, like accidents or falls, can hurt the urethral tissues7. This is a common cause.
Medical procedures, like catheter use and prostate surgery, can also cause scarring. Over 2% of prostate cancer patients get urethral strictures from radiation8.
Inflammatory conditions, like STIs and balanitis xerotica obliterans, can lead to chronic inflammation. This can cause urethral strictures7.
In about 30% of cases, the exact cause is unknown8. While men are more likely to get urethral strictures because of their longer urethra8, women and children can also be affected, though less often8.
| Cause | Percentage |
|---|---|
| Traumatic Injuries | Varies |
| Medical Procedures | Over 2% for prostate cancer patients |
| Inflammatory Conditions | Varies |
| Unknown | 30% |
Knowing the causes and risk factors is key to preventing and managing urethral stricture disease. Healthcare providers can then tailor treatments to each patient’s needs7.
Symptoms and Clinical Manifestations
People with urethral stricture disease face many urinary symptoms. A slow or weak urine stream is common910. They might feel the need to urinate often, with pain and bleeding. The fear of urinating can be overwhelming10.
Some struggle to empty their bladder, leading to discomfort10. Untreated strictures can lead to serious issues like infections and bladder damage10. Women can also get strictures, showing similar symptoms10.
Symptoms can range from mild to severe, even causing complete urinary retention9. About 1% of men in the U.S. have this condition11. If not treated, it can greatly affect a person’s life quality.
| Symptom | Description |
|---|---|
| Slow/Weak Urine Stream | Urethral strictures can cause a slow, weak, or interrupted urine stream, making it difficult to completely empty the bladder. |
| Frequent Urination | Patients may experience an urgent and frequent need to urinate, even when the bladder is not completely full. |
| Pelvic Pain | Some individuals with urethral strictures may experience discomfort or pain in the pelvic region, particularly during urination. |
| Urinary Retention | In severe cases, urethral strictures can lead to complete or near-complete blockage of urine flow, resulting in urinary retention. |
| Urinary Tract Infections | Untreated urethral strictures can increase the risk of recurrent urinary tract infections. |
It’s important to recognize and treat urethral stricture disease symptoms. This helps in diagnosing and treating the condition effectively. Healthcare providers can then create a treatment plan tailored to each patient, improving their urinary health and quality of life91011.
Diagnostic Approaches and Evaluation Methods
Getting a correct diagnosis is key to managing urethral stricture disease well. Doctors use many methods to check the stricture’s location, length, and how bad it is. These include imaging, physical checks, and special urology tests.
Imaging Techniques
The retrograde urethrogram is a big help. It uses dye and X-rays to see the stricture. Urethroscopy lets doctors look inside the urethra with a thin tool. Cystoscopy uses a camera to check the bladder. These tools give doctors the info they need to plan treatment12.
Physical Examination
A detailed physical check is also important. Doctors feel the urethra and genital area. This helps them see how big the stricture is and if there are other problems13.
Urological Tests
Tests like urine flow studies and ultrasound help too. They check how well urine flows and if there’s urine left in the bladder. This info helps doctors choose the best treatment1213.
By using these methods together, doctors can really understand the stricture. Then, they can make a treatment plan that fits the patient’s needs.
| Diagnostic Approach | Key Findings | Clinical Significance |
|---|---|---|
| Retrograde Urethrogram | Visualization of the stricture location and length | Guides treatment planning and decision-making |
| Urethroscopy | Direct inspection of the urethra and stricture | Allows for assessment of stricture characteristics and presence of other pathologies |
| Cystoscopy | Evaluation of the bladder and lower urinary tract | Helps identify any underlying or associated conditions |
| Urine Flow Studies | Measurement of urine flow rate and pattern | Assesses the functional impact of the stricture on urinary function |
| Ultrasound Imaging | Evaluation of bladder and post-void residual urine | Provides additional information on the stricture’s effects on the urinary tract |
Using all these methods helps doctors understand the stricture well. They can then make a treatment plan that’s just right for each patient1213.
Urethral Stricture Disease: Prevalence and Demographics
Urethral stricture disease (USD) is a common issue, especially for men. This is because men have longer urethras. In the U.S., over 5,000 men are admitted to the hospital each year for this condition. More than 1.5 million men visit healthcare providers for it14.
USD mostly affects men over 65. It impacts about 0.6% of all men14.
While men get urethral strictures more often, women can also be affected. However, it’s much rarer in women. Women face unique challenges in getting diagnosed and treated for this condition14.
The number of people with USD has gone up since the early 2000s. The cost of treating USD in the U.S. is estimated to be up to $200 million each year14.
| Characteristic | Value |
|---|---|
| Prevalence of USD in men | 0.6% |
| Annual hospital admissions for male USD | Over 5,000 |
| Annual healthcare visits for male USD | Over 1.5 million |
| Healthcare expenditure related to USD treatment | Up to $200 million per year |
The rising number of cases and costs show we need better treatments. The Optilume procedure is a new option. It aims to improve how we manage USD and help patients1415.
Traditional Treatment Methods
Traditional treatments for urethral stricture disease include urethral dilation procedures and direct vision internal urethrotomy (DVIU)16. These methods are used often but work well in less than half the cases, especially for those with recurring issues16.
In a dilation procedure, doctors use special tools or balloons to stretch the narrowed urethra. Urethral catheterization is another method, where a tube is placed in the urethra to improve urine flow17. The sizes of these balloons range from 18Fr to 36Fr, with the 36Fr size approved only in the U.S17..
DVIU involves cutting scar tissue endoscopically to widen the area. It’s used for shorter, less severe strictures. Yet, it has a high failure rate, with only about 20% of patients staying stricture-free long-term16. Urethroplasty is seen as the best treatment, with a success rate of 90%16.
| Treatment Method | Success Rate |
|---|---|
| Urethral Dilation/DVIU | Less than 50% |
| Urethroplasty | 90% |
“Optilume technology provides superior outcomes compared to standard endoscopic management according to clinical data.”17
Advanced Surgical Options for Urethral Reconstruction
For those with complex or recurring urethral strictures, advanced surgery like urethroplasty offers hope. Urethroplasty is the top choice for tough strictures. It uses various methods based on the patient’s needs.
Urethroplasty Techniques
Short strictures often get the EPA treatment. This means removing the bad part and joining the good ends18. It works well for strictures up to 4 cm long, with a success rate of 95%18.
For longer or more complex strictures, tissue grafts are used18. The buccal mucosal graft, taken from the cheek, is a top choice. It’s known for its durability and success rate of 80-85% for repairs18.
Tissue Grafting Options
Buccal mucosa grafts are becoming more popular for urethral repairs19. They’re reliable and effective, with success rates similar to other methods. They also have a lower chance of causing incontinence after surgery19.
Other grafts like full-thickness skin and acellular bladder matrix also work well in certain cases18. The right graft depends on the patient’s situation and the surgeon’s skills.
Urologists use the latest in urethroplasty and grafting to help patients with urethral strictures20. These advanced methods, along with the help of top places like Mayo Clinic, bring hope and better lives to those affected20.
Minimally Invasive Procedures

Minimally invasive procedures are now seen as good alternatives to open surgery for urethral stricture disease21. Techniques like urethral stent placement and visual internal urethrotomy are less invasive. They can lead to faster recovery times21.
These endoscopic procedures are used for short, less severe strictures or when other surgeries are not suitable21. They aim to widen the narrowed urethra and improve urine flow. However, they might have a higher chance of the stricture coming back compared to bigger surgeries21.
Choosing between a minimally invasive procedure and a bigger surgery depends on the stricture’s details, the patient’s health, and the surgeon’s advice21. It’s important for patients to talk to their urologist. They need to understand the benefits, risks, and recovery times of each option. This helps them make a choice that fits their needs and preferences.
In recent years, the FDA has approved new treatments like the Optilume® Drug Coated Balloon2223. It combines dilation with a drug to prevent stricture recurrence2223. This method has shown good results in studies, offering a new hope for avoiding big surgeries2223.
As we move forward, more minimally invasive treatments will be available for urethral stricture management212223. These options aim to provide lasting solutions with less invasive methods212223.
The Revolutionary Optilume Treatment
If you’re dealing with a urethral stricture, Optilume might be the answer. It’s a drug-coated balloon catheter that dilates the urethra and delivers medication. This new method changes how we treat urethral strictures.
How Optilume Works
The Optilume device expands the urethra while releasing paclitaxel. This medicine stops cells from growing and forming scars. It’s a new way to prevent strictures from coming back, unlike old methods24.
Patient Selection Criteria
Optilume works well for short bulbar urethral strictures, with a 70% success rate at 12 months24. But, choosing the right patient is key. Your doctor will check if you fit the criteria for this advanced treatment.
Optilume is best for short, proximal urethral strictures. Your doctor will look at your stricture’s location and size. They’ll also consider other factors to see if Optilume is right for you.
Optilume is a new, exciting option for treating urethral stricture disease1. It combines dilation with drug delivery for lasting relief. This could greatly improve your life if you have this condition.
If you’re thinking about Optilume, talk to a skilled urologist. They can give you advice tailored to your health needs1.
Post-Treatment Care and Recovery
The recovery time after urethral surgery can differ based on the procedure. More complex surgeries, like urethroplasty, might need longer hospital stays and catheter use for weeks25. On the other hand, simpler procedures, like urethral dilation, can have quicker recovery times. Most people can get back to their daily activities in 1-2 days25.
After surgery, doctors watch for any complications and signs of urethral strictures coming back. They use tests and scans to check if the treatment worked25. They also give detailed instructions on managing medications, especially blood thinners like aspirin, to help with recovery25.
The Optilume® treatment has a generally smooth recovery process26. It’s used for treating urethral strictures up to 3 cm in adult males26. Some patients might feel mild discomfort or soreness in the urethra, but this usually goes away in a day or two25. By following the doctor’s advice and staying healthy, most people can get back to their normal life quickly.
It’s important to keep a healthy lifestyle, drink plenty of water, and follow the doctor’s post-treatment instructions. This helps ensure a good recovery and avoids future problems25.
“Proper post-treatment care is essential for a successful recovery and the prevention of future complications.”
Prevention Strategies and Lifestyle Modifications
To prevent urethral stricture disease, we need to take several steps. Keeping the area clean and avoiding injuries to the pelvic area are key27. In rich countries, most strictures come from medical procedures. In poorer areas, infections and injuries are more common27.
Treating urinary tract infections quickly can stop strictures from forming28. If strictures do happen, they often come back within a few months28. Using careful techniques when using catheters can also help avoid injuries.
Changing your lifestyle can help too. Avoiding sports or activities that might hurt your pelvic area is important28. For short strictures, removing and reconnecting the urethra works well. It keeps the urethra open and has few side effects28.
- Practice good hygiene to reduce the risk of urinary tract infections.
- Avoid activities that could lead to pelvic trauma, such as contact sports.
- Seek prompt treatment for any urinary tract infections or inflammatory conditions.
- Follow proper catheterization techniques to minimize the risk of iatrogenic urethral injury.
By following these steps and making lifestyle changes, you can lower your risk of urethral stricture disease27. Studies show that simple balloon dilation can work for 67.07% of male urethral strictures27.
“Urethral stricture disease is a complex condition that requires a comprehensive approach to prevention and management. By addressing the underlying risk factors and adopting appropriate lifestyle modifications, individuals can take proactive steps to maintain their urinary health.”
Special Considerations for Different Patient Groups
Treating urethral strictures can vary based on the patient’s situation. Elderly patients or those with health issues might need less invasive methods to avoid surgery risks29. On the other hand, those with recurring strictures might need more complex surgeries to fix their condition29.
Women with urethral strictures are a special case because it’s rare in them due to their anatomy30. They might need special treatments to fix their unique problems and get back to normal.
For men with BPH, treatment choices depend on how symptoms affect their life. Usually, doctors start with medicine29. A mix of medicines can greatly improve symptoms in the short and long term29. If medicine doesn’t work or causes side effects, surgery might be considered, like TURP, which is the standard29.
New treatments like the iTind nitinol device or the Optilume® BPH Catheter System are being looked at for BPH symptoms29. These options aim to help patients without the usual risks and help them recover faster.
Every patient’s treatment plan for urethral strictures is unique. It depends on their age, health, and how serious their condition is. By choosing the right treatment for each patient, doctors can help them get the best results293018.
Conclusion
Treatment for urethral stricture disease has made big strides. Now, patients have many options, from simple procedures to complex surgeries. The right treatment depends on the stricture’s type, the patient’s health, and the surgeon’s skills22.
New technologies, like the Optilume drug-coated balloon, are showing great promise. They’ve led to better results for patients with urethral strictures. For example, studies found a 75% success rate at 6 months and a 68% success rate at 2 years. This success rate even stayed at 67% after 3 years31.
Research is still going on to make treatments even better. This includes using new methods like regenerative medicine. Thanks to advances in minimally invasive techniques and new tools like Optilume, treating urethral strictures is getting better. This means patients have a good chance of feeling better and living better lives32.
FAQ
What is a urethral stricture?
A urethral stricture is when the urethra gets narrower because of scar tissue. This makes it hard to empty the bladder and can cause lasting damage.
What are the common causes of urethral strictures?
Strictures can happen from injuries, medical procedures, or infections like STIs and Lichen sclerosis.
What are the symptoms of urethral stricture disease?
Symptoms include a slow urine stream, needing to urinate often, and trouble starting to urinate. You might also feel pain or see blood when you pee. Other signs are abdominal pain, discharge, and losing bladder control.
How are urethral strictures diagnosed?
Doctors use physical checks, imaging like retrograde urethrogram, and tests like urethroscopy and urine flow tests. These help find where, how long, and how bad the stricture is.
What are the traditional treatments for urethral strictures?
Old treatments include dilation and direct vision internal urethrotomy (DVIU). These stretch or cut the scar tissue. They work for short, mild strictures but often need to be done again.
What is the gold standard for treating complex or recurrent urethral strictures?
Urethroplasty is the best treatment for tough or recurring strictures. It involves removing the scar tissue and reconnecting the urethra. Sometimes, grafts like buccal mucosa grafts are used.
What are some of the minimally invasive procedures for urethral strictures?
Less invasive options include endoscopic techniques and stent placement. These are less invasive than surgery but might not work as well.
What is Optilume, and how does it work?
Optilume is a new drug-coated balloon catheter. It stretches the urethra and releases paclitaxel to stop scar tissue. It shows promise for treating short strictures.
What are some considerations for post-treatment care and recovery?
Care after treatment depends on the method used. Urethroplasty patients might need to stay in the hospital and use a catheter for weeks. Minimally invasive methods have quicker recovery times. Patients are watched for any problems or if the stricture comes back.
Are there any prevention strategies for urethral strictures?
To prevent strictures, keep clean to avoid infections, avoid injuries, and use catheters carefully. Treating infections and conditions quickly can also help prevent strictures.
Source Links
- Optilume – Z Urology – https://zurology.com/optilume/
- A drug-coated balloon treatment for urethral stricture disease: Two-year results from the ROBUST I study – https://pmc.ncbi.nlm.nih.gov/articles/PMC7864702/
- Urethral Strictures – StatPearls – NCBI Bookshelf – https://www.ncbi.nlm.nih.gov/books/NBK564297/
- Optilume for Urethral Strictures – University Urology Associates – https://uuaurology.com/treatments-and-procedures/optilume-for-urethral-strictures/
- Practice Essentials, Relevant Anatomy, Pathophysiology – https://emedicine.medscape.com/article/450903-overview
- Medical Student Curriculum: Urethral Strictures – https://www.auanet.org/meetings-and-education/for-medical-students/medical-students-curriculum/urethral-strictures
- Urethral stricture: MedlinePlus Medical Encyclopedia – https://medlineplus.gov/ency/article/001271.htm
- Urethral Stricture Treatments & Information – https://www.laborie.com/blog/2023/04/12/urethral-stricture-treatment/
- Urethral Stricture – https://www.uclahealth.org/medical-services/womens-pelvic-health/conditions-treated/urethral-stricture
- Urethral Stricture Diagnosis & Treatment | Mount Sinai – https://www.mountsinai.org/care/urology/services/reconstructive-urology/urethral-strictures
- Redefining the male urethral stricture treatment paradigm – https://www.mayoclinic.org/medical-professionals/urology/news/redefining-the-male-urethral-stricture-treatment-paradigm/mac-20463849
- A single-institution experience with the Optilume Urethral Drug Coated Balloon for management of urethral stricture disease – https://pmc.ncbi.nlm.nih.gov/articles/PMC11399038/
- Urethral Stricture – AUA Guideline – https://www.auanet.org/guidelines-and-quality/guidelines/urethral-stricture-guideline
- Frontiers | Therapeutic adjuncts in the endoscopic management of urethral stricture disease: past, present, and future – https://www.frontiersin.org/journals/urology/articles/10.3389/fruro.2024.1342941/full
- Balloon dilation for the treatment of male urethral strictures: a systematic review and meta-analysis – https://bmjopen.bmj.com/content/14/2/e071923
- JU-21-1904_pap 1..9 – https://urology.wisc.edu/wp-content/uploads/2022/02/Optilume.pdf
- Optilume® for Urethral Stricture | Urethral Drug Coated Balloon – https://www.laborie.com/product/optilume-drug-coated-balloon-for-urethral-stricture-treatment/
- Approach Considerations, Surgical Therapy, Open Reconstruction – https://emedicine.medscape.com/article/450903-treatment
- Posterior Urethral Stenosis (PUS) After Prostate Cancer Therapy – https://grandroundsinurology.com/posterior-urethral-stenosis-pus-after-prostate-cancer-therapy/
- Urethral stricture – Care at Mayo Clinic – https://www.mayoclinic.org/diseases-conditions/urethral-stricture/care-at-mayo-clinic/mac-20362386
- Urethral stricture treatment using Optilume® technology | Top Doctors – https://www.topdoctors.co.uk/medical-articles/using-optilume-for-urethral-stricture-treatment
- Optilume drug‐coated balloon for anterior urethral stricture: 2‐year results of the ROBUST III trial – https://pmc.ncbi.nlm.nih.gov/articles/PMC10927926/
- mp-761 – Medical Policies – Liferay – https://mn-policies.exploremyplan.com/portal/web/medical-policies/-/mp-761
- Recent Advances in treatment of urethral stricture disease in men – https://pmc.ncbi.nlm.nih.gov/articles/PMC7202089/
- What to Expect at Home – https://myhealth.alberta.ca/Health/aftercareinformation/pages/conditions.aspx?hwid=acg6151
- Microsoft Word – P210020-A003 – Urotronic-Optilume – SSED – FINAL-v8.docx – https://www.accessdata.fda.gov/cdrh_docs/pdf21/P210020B.pdf
- Balloon dilation for the treatment of male urethral strictures: a systematic review and meta-analysis – https://pmc.ncbi.nlm.nih.gov/articles/PMC10860052/
- Management of urethral strictures – PMC – https://pmc.ncbi.nlm.nih.gov/articles/PMC2585709/
- Devices for Treatment of Benign Prostatic Hyperplasia, Urethral Stricture, and Urethral Stenosis – https://beonbrand.getbynder.com/m/947bd9ec51381650/original/Devices-for-Treatment-of-Benign-Prostatic-Hyperplasia-Urethral-Stricture-and-Urethral-Stenosis.pdf
- EAU Guidelines on Urethral Strictures – Uroweb – https://uroweb.org/guidelines/urethral-strictures/chapter/references
- Dr. Chee summarizes latest Optilume data in patients with urethral strictures – https://www.urologytimes.com/view/dr-chee-summarizes-latest-optilume-data-in-patients-with-urethral-strictures
- Optilume drug-coated balloon for anterior urethral stricture: 2-year results of the ROBUST III trial – https://experts.umn.edu/en/publications/optilume-drug-coated-balloon-for-anterior-urethral-stricture-2-ye